Updated: New Model Forecasts When States Likely to See Peak in COVID-19
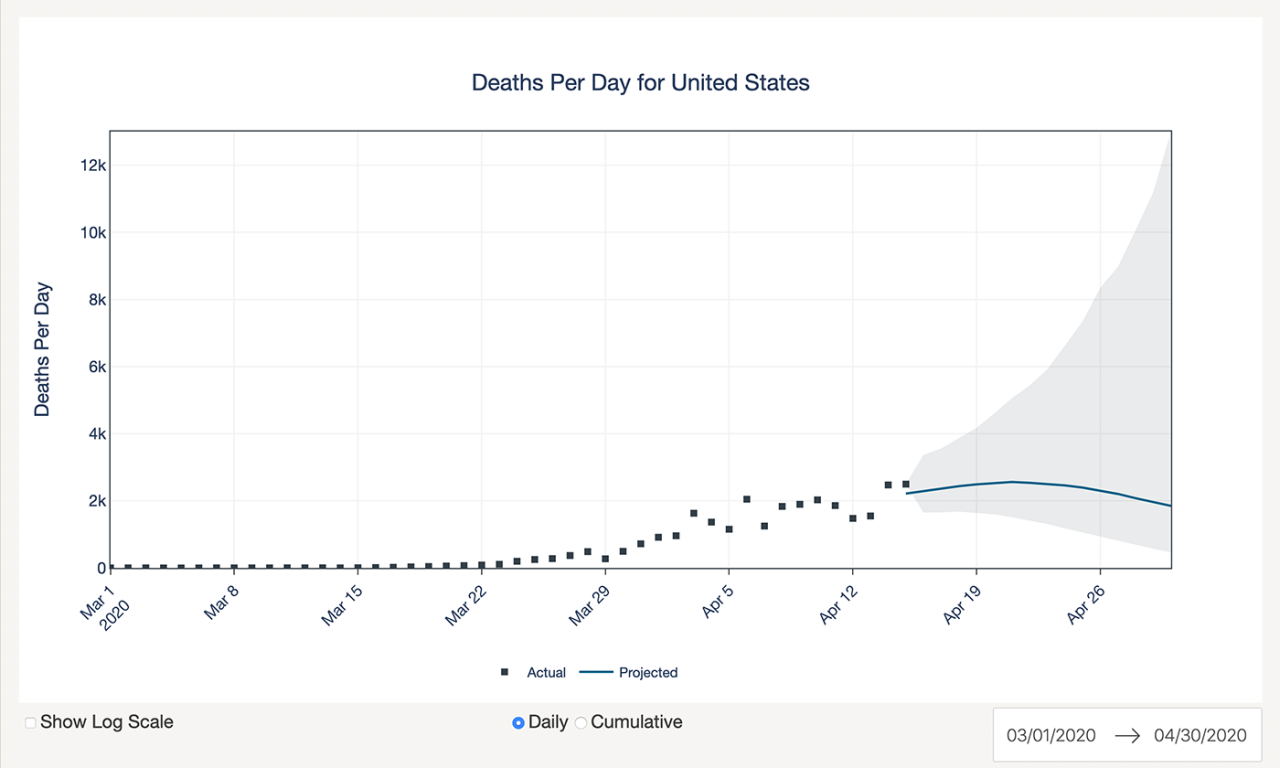
A computer model from the UT COVID-19 Modeling Consortium forecasts daily deaths from COVID-19 for the entire US and each state. Credit: University of Texas at Austin.
The following is based on an original article by Marc Airhart
A model that projects COVID-19 deaths for all 50 U.S. states using geolocation data from cellphones to determine the impact of social distancing within each state is showing it may be another several weeks until deaths peak for many states.
Researchers at The University of Texas at Austin have released a model that provides a daily estimate of fatalities from COVID-19 in the United States for the coming weeks. As of April 17, the UT model finds that the number of deaths almost certainly has not yet peaked and is not likely to peak in many states until after May 1, a finding that is in contrast to one of the most frequently cited models.
The UT model has several similarities with a model developed by the University of Washington's Institute for Health Metrics and Evaluation (IHME), but it stands in contrast because it uses data from the United States to estimate the impact of recent social distancing measures within each state.
The UT model predicts that two states, New York and Louisiana, will be past their peak by April 19 with at least 80% certainty. The model also predicts that 7 others, plus Washington, D.C., have at least an 80% chance of peaking in April: New Jersey, Michigan, Colorado, Connecticut, Florida, Nevada and Massachusetts. For the whole U.S., the IHME model predicts deaths already peaked on April 13, whereas the new model predicts that there is an 80% chance that the U.S. will have peaked by May 7, and only a 17% chance that the peak has already passed. [Update: As new data on deaths become available projections are updated. For the latest projections, please visit this website.]
The team is providing the new model to the Centers for Disease Control and Prevention and the White House Coronavirus Task Force, and is presenting it to the public and decision makers in advance of scientific peer review due to the time-sensitive nature of the subject. For detailed technical information please view the Report: UT COVID-19 Mortality Forecasting Model.
The model was developed by several UT Austin researchers: professor James Scott and professor Lauren Ancel Meyers, who leads the UT COVID-19 Modeling Consortium; graduate students Spencer Woody and Mauricio Garcia Tec; research associate Spencer Fox; and professor Kelly Gaither and Maytal Dahan, both with UT Austin's Texas Advanced Computing Center. Professor Michael Lachmann of the Santa Fe Institute also contributed to the work.
"On average, there seems to be a 3-4 week lag between when someone gets infected with COVID-19 and when they're at risk of death," Meyers said. "That means we're just beginning to see the life-saving benefits—and the clear signal in the data—of social distancing that began in mid- to late March."
The UT model tracks the local impact of social distancing through GPS traces from tens of millions of mobile phones. The cellphone data, aggregated and anonymized, reflect how often people congregate in public places such as restaurants, bars, schools, parks, pharmacies and grocery stores, as well as the amount of time people spend at work versus at home. The researchers found clear evidence that the timing and extent of people's distancing behavior differ across states—and that these differences matter in terms of "flattening the curve." In Texas, for example, many large cities issued stay-at-home orders that began to curtail mobility many days before a statewide policy was enacted.
The IHME model is widely used across the U.S. by decision makers and the health care industry and relies heavily on patterns of reported deaths in other parts of the world, including Wuhan, China, where social distancing measures differ from the U.S. Using the new geolocation data, the UT Austin model projects different numbers of COVID-19 daily deaths in the coming weeks compared with the IHME model. For example, on April 30 it predicts far more deaths than the IHME model in Illinois (75 vs. 2) and Pennsylvania (134 vs. 35).
In addition to using local movement data from individual U.S. states to make projections rather than drawing on patterns observed in other countries, another difference in the UT researchers' model is that it accounts for greater uncertainty further in the future. Recent updates of the IHME model have resulted in large swings in the projected numbers of COVID-19 deaths. In some cities, the forecasted peaks have changed by more than a factor of 10, yet the confidence intervals in the IHME projections show near certainty regarding the number of COVID-19 deaths that will occur six weeks from now.
By accounting for more sources of uncertainty, the UT model projects a greater range of plausible COVID-19 deaths than the IHME model. In Wisconsin, for example, the UT model predicts that there could be anywhere from 0 to 89 deaths on May 1, whereas IHME predicts a maximum of 5 deaths; likewise the UT model caps May 1 deaths at 71 for Colorado, whereas IHME projects no more than 6.
"While more uncertain forecasts may be disconcerting, we believe that they reflect the true range of possibilities that could unfold in the weeks ahead," Scott said. "Our model stands on the shoulders of the IHME model, but it corrects critical statistical flaws that led the IHME model to make many projections that, in retrospect, have turned out to be far too optimistic."
The research was published today by the UT COVID-19 Modeling Consortium and the Texas Advanced Computing Center, which hosts the projections on a new website: https://covid-19.tacc.utexas.edu/projections/